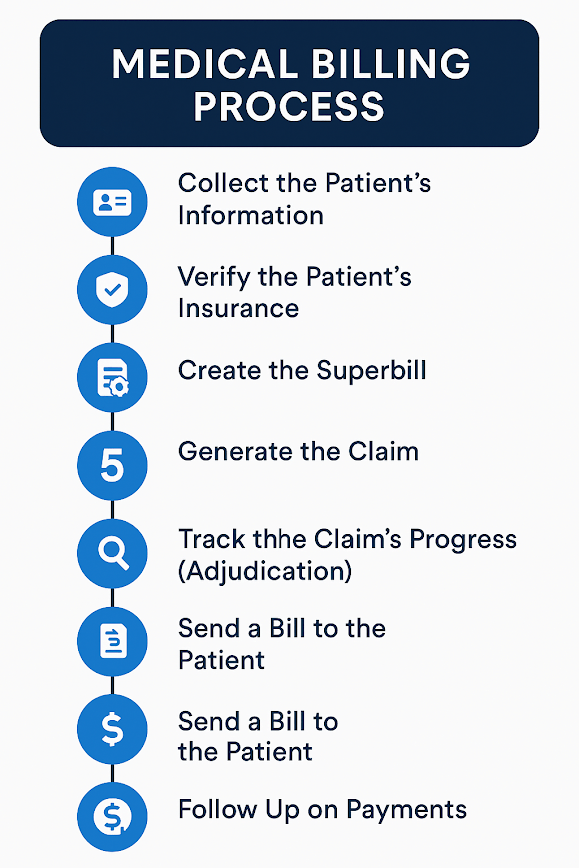
The medical billing process is how doctors and healthcare providers get paid for the care they provide to patients. Aside from treating patients, it’s one of the most important parts of keeping a medical office running smoothly.
This guide will walk you through the medical billing process steps for quick reference.
If you’re a healthcare provider—whether you’re a doctor, pharmacist, or therapist—it’s important to understand how billing works so you can make sure you’re getting paid properly for your work.
What Is the Medical Billing Process?
Medical billing is everything that happens from when a patient is first registered to when the doctor gets paid for the care they provided. It involves the patient, the healthcare provider, and the insurance company. These three parties need to communicate and share information throughout the process.
This whole process is also called the billing cycle. How long it takes to finish one billing cycle can tell you how well your office is doing.
On average, it takes about 40 to 50 days for most medical offices to complete a billing cycle. Some efficient practices manage to do it in 30 days or less. How does your office compare?
There are ways to make the billing process in healthcare faster. For example, you can:
- Improve how often your insurance claims get approved on the first try.
- Use billing software to make the process smoother.
- Speeding up your billing cycle is helpful because the faster you get paid, the more steady your cash flow will be.
But before we talk about how to make it faster, let’s first go over each step in the billing process.
What Are The Steps Involved In The Medical Billing Process And Procedures?
1. Collect the Patient’s Information
When a new patient calls to make an appointment, your front desk will ask for basic info like their name, age, insurance details, and contact info. This is the first step in billing — getting all the right information upfront.
If it’s a returning patient, you don’t need to re-enter everything. Just check their existing file and update anything that’s changed, like a new phone number or insurance card.
2. Verify the Patient’s Insurance
Once you have their insurance info, call the insurance company to make sure it’s still valid. The number is usually on the back of their insurance card.
Ask questions like:
- Is this insurance plan still active?
- What services are covered?
- How much is the patient’s deductible or co-pay?
Knowing this helps avoid billing surprises later.
3. Create the Superbill
When the patient comes in for their visit, ask them to:
- Confirm or update their information,
- Show proof of ID and insurance,
- And pay their co-pay if needed.
After the appointment, a medical coder looks at the doctor’s notes and turns them into billing codes for what was done and why.
All this info goes into something called a superbill, which includes:
- Info about the doctor and clinic,
- Patient details and medical history,
- Services provided,
- Diagnosis and procedure codes.
4. Generate the Claim
Now that you have the superbill, the billing team creates a medical claim to send to the patient’s insurance company. Before sending, double-check it to make sure the codes and format are correct and meet HIPAA and insurance rules.
5. Submit the Claim
Once the claim looks good, it’s sent to the insurance company. Most of the time, this is done electronically through a third-party service, which helps handle communication between your office and the insurance company. Some big payers may accept claims directly.
6. Track the Claim’s Progress (Adjudication)
The insurance company will now review the claim. This is called adjudication. They check if everything looks correct and whether the services are covered.
They’ll then:
- Approve the claim and pay your office,
- Deny the claim (but you can fix it and send it again),
- Or reject it (if it’s missing important info).
7. Send a Bill to the Patient
If the insurance doesn’t cover the whole cost, you’ll send the patient a statement showing:
- What services did they receive?
- How much did the insurance pay?
- How much do they still owe?
This helps the patient understand exactly what they’re being charged for.
8. Follow Up on Payments
Once the claim is approved, wait for the payment to come in. Sometimes this takes a while. Keep track of which claims haven’t been paid yet. If a payment is taking too long, follow up with the insurance company until it’s resolved.
Tips for a Smoother Medical Billing Process (in Plain Language)
Understand the Process First
Before you try to fix billing problems, make sure you understand how to do medical billing. Think of it this way: you can’t solve a problem if you don’t know what’s causing it.
The medical billing process usually has six basic steps:
- Check if the patient’s insurance is active
- Collect what the patient owes (co-pays, deductibles, etc.)
- Use the right procedure and diagnosis codes for their visit
- Make sure those codes are correct
- Enter the claim into your billing software
- Get paid by the insurance company
Don’t Make Assumptions
It’s important to never assume a patient knows what they owe. A lot of patients are confused about what their insurance covers. Some don’t know how much their co-pay or deductible is, which can lead to missed payments.
Use the Right Billing Method
To keep money flowing in, use a simple and consistent system for billing. The best method? Usually electronic billing.
Avoid using multiple ways to collect payment (like mailing bills, calling patients, and sending them to collections all at once). That just causes confusion and delays. Instead, be clear and consistent.
Helpful Tips to Avoid Billing Problems
- Find out the patient’s billing in healthcare before their appointment.
- Remind patients of what they’ll need to pay at every visit.
- If any procedures need pre-approval from insurance, take care of it early.
- Be clear about your billing policies and display them in your office.
- Post signs reminding patients that payment is expected at the time of service.
The “Big Three” for Billing Success
To avoid losing money, focus on these three things:
- Knowledge – Learn the full billing process and stay updated.
- Mentorship – Teach your coworkers so the whole team is strong.
- Practice – Keep refining the process and fixing mistakes.
Most billing delays are caused by simple errors that can be prevented with a well-trained team.
Watch Out for Common Mistakes
Small errors can cause big billing problems. Here are some of the most common issues in insurance claims:
- Wrong name or birthdate for the patient
- Wrong address or phone number for your clinic
- Incorrect insurance details (like policy number or payer ID)
- Messy, handwritten notes that are hard to read
- Missing claim numbers when submitting appeals
- Paying attention to details helps prevent these mistakes and keeps your payments on track.
Why Should Medical Assistants Learn Medical Billing?
It’s a great idea for Medical Assistants (MAs) to learn healthcare billing management. Why? Billing is a big part of keeping a medical office running smoothly and financially healthy.
When MAs, Medical Office Assistants (MOAs), and billing staff handle these tasks, doctors can spend more time focusing on patients.
Even though medical billing isn’t always required in the job description, MAs are often asked to help with it. It’s a useful and practical skill that can open doors to more career opportunities.
If you’re a Medical Assistant or training to become one, learning billing can:
- Make you more valuable to your employer
- Help you stand out at work
- Lead to more responsibilities and career growth
So, getting trained in medical billing is a smart move!
Program Offered
- Pharmacy Technician Training
- Online Medical Assistant
- Medical Billing and Coding Specialist Program
- Cloud Computing Technician Training
- Computer Network Technician
- Business and Accounting
- Radiology Technician Training
- Medical Assistant Program
- Computer Support Technician
- Cybersecurity Program
- Virtual Assistant Training
This article is written by
Share this article
Program Offered
- Pharmacy Technician Training
- Online Medical Assistant
- Medical Billing and Coding Specialist Program
- Cloud Computing Technician Training
- Computer Network Technician
- Business and Accounting
- Radiology Technician Training
- Medical Assistant Program
- Computer Support Technician
- Cybersecurity Program
- Virtual Assistant Training
This article is written by
Share this article
Related Articles





CCI Training Center Proudly Completes
41 Years in Career Training Services