Summary
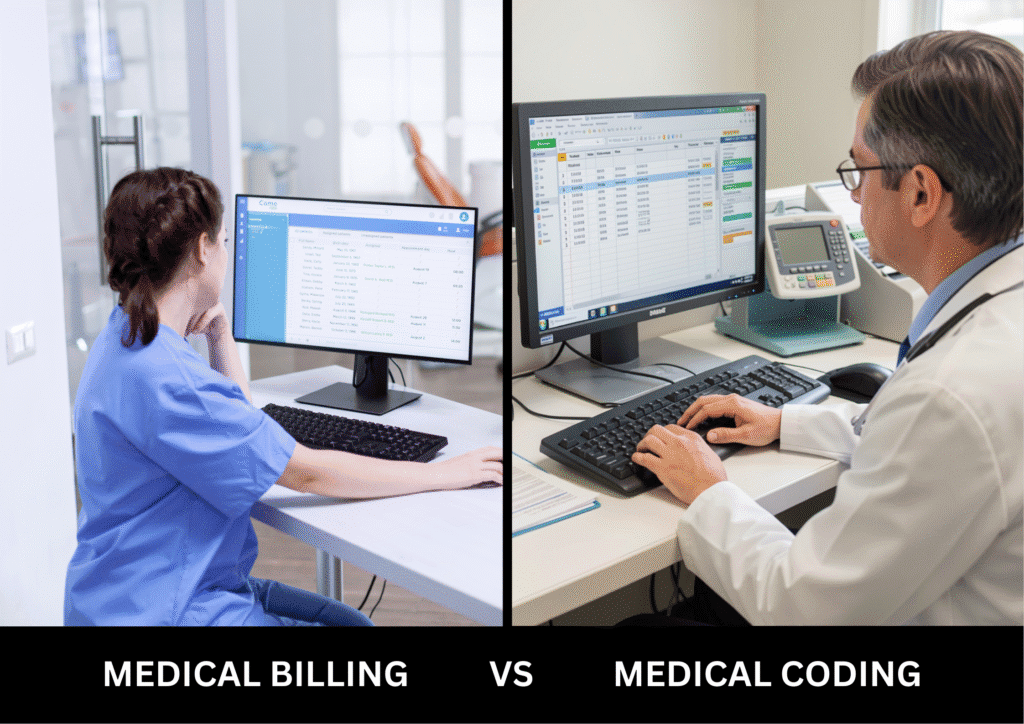
Looking to build a fulfilling career in healthcare administration? Then, becoming a medical coder or biller might be a great option for you, as these are fundamental healthcare administrative processes. Although these roles are interconnected, they serve different purposes, with each requiring unique skills and responsibilities.
This blog will help you choose the right career.
Quick Summary
|
What Does a Medical Biller Do?
A medical biller submits and follows up on claims with health insurance companies to receive payments for services provided by healthcare providers. Being a medical biller, you’d also need to ensure that healthcare providers are compensated for their services in a timely manner. A typical medical billing process involves:
- Patient Registration: Collecting personal and insurance information.
- Charge Entry: Entering services (like consultation or medical exam) provided into the billing system.
- Claim Submission: Sending claims to insurance companies for reimbursement.
- Payment Posting: Recording payments received and reconciling accounts.
How to Become a Medical Biller in the US?
Here’s how to become a medical biller in 6 easy steps:
- Step 1: Understand the Role: First things first, you’d need to understand the niche of medical billing and if it’s a right fit for you.
- Step 2: Meet Educational Requirements: While different states have different education requirements for a medical biller, you’d need a high school diploma or GED at the very least.
- Step 3: Complete Specialized Training: Enroll yourself in an accredited medical billing course by a trusted platform like CCI Training Center.
- Step 4: Gain Practical Experience: Apply for internships to apply your knowledge in real-world settings.
- Step 5: Get Certified: While CCI Training Center provides you with a certification, it’s still a good idea to get additional certifications like the Certified Professional Biller (CPB) to enhance your job prospects.
- Step 6: Apply for a Job: Once you’ve completed all the mentioned steps, you can apply for a medical billing job by searching job boards like Indeed, LinkedIn, and more.
How Much Does a Medical Biller Earn?
In the United States, the average salary of a medical biller is $37,421 per year.
What Does a Medical Coder Do?
A medical coder is a person who translates healthcare diagnoses, procedures, and services into standardized codes. These codes are then used by insurance companies to understand exactly what happened during the visit or procedure. Typically, medical codes are primarily derived from two coding systems:
- ICD-10 (International Classification of Diseases, 10th Revision): Utilized to code diagnoses.
- CPT (Current Procedural Terminology): Used for coding medical procedures and services.
How to Become a Medical Coder in the US?
Here’s how to get ready for a medical coding position in just six easy steps:
- Step 1: Understand the Role: Similar to medical billing, you’d need to understand all the hows and whys of this job role.
- Step 2: Meet Educational Requirements: You’d need to have a high school diploma or GED at the very least.
- Step 3: Complete Specialized Training: Get specialized medical coding training from an accredited platform. Here, you’d need to learn ICD-10 and CPT, along with medical terminology.
- Step 4: Gain Practical Experience: Apply for internships to apply your knowledge in real-world settings.
- Step 5: Get Certified: While CCI Training Center provides you with a Certified Professional Coder (CPC) Certification, you can always add more to your portfolio.
Step 6: Apply for a Job: Once you’ve completed all the mentioned steps, you can apply for a medical coding job by searching job boards like Indeed, LinkedIn, and more.
How Much Does a Medical Coder Earn?
As of 2025, the average annual salary for an entry-level medical coder in the United States is $39,975.
Key Differences Between Medical Billing and Medical Coding?
| Aspect | Medical Billing | Medical Coding |
| Main Role | Financial process of submitting and tracking claims. | Translating healthcare diagnoses and procedures into standardized codes. |
| Skills Required | Knowledge of insurance policies, payment processes, and medical billing software. | Knowledge of medical terminology, anatomy, and coding systems (ICD-10, CPT). |
| Type of Work | Manages billing cycle, claim submission, and payment posting. | Assign codes to diagnoses and procedures from medical records. |
| Job Goal | To ensure accurate and timely reimbursement for services rendered. | To ensure proper coding for diagnoses and procedures, ensuring accuracy in billing. |
| Tools Used | Billing software, insurance forms, patient records. | Coding manuals, coding software, medical records. |
Medical Billing vs. Medical Coding: Which Is Right for Me?
While medical coding and medical billing work closely in the healthcare system, these are two distinct roles.
So, if you wish to translate small details of a medical visit into codes, then it’s best to aim for medical coding. On the other hand, if you wish to involve yourself with billing and payments, then medical billing is the right choice for you.
Program Offered
- Pharmacy Technician Training
- Online Medical Assistant
- Medical Billing and Coding Specialist Program
- Cloud Computing Technician Training
- Computer Network Technician
- Business and Accounting
- Radiology Technician Training
- Medical Assistant Program
- Computer Support Technician
- Cybersecurity Program
- Virtual Assistant Training
This article is written by
Share this article
Program Offered
- Pharmacy Technician Training
- Online Medical Assistant
- Medical Billing and Coding Specialist Program
- Cloud Computing Technician Training
- Computer Network Technician
- Business and Accounting
- Radiology Technician Training
- Medical Assistant Program
- Computer Support Technician
- Cybersecurity Program
- Virtual Assistant Training
This article is written by
Share this article
Related Articles







CCI Training Center Proudly Completes
41 Years in Career Training Services










