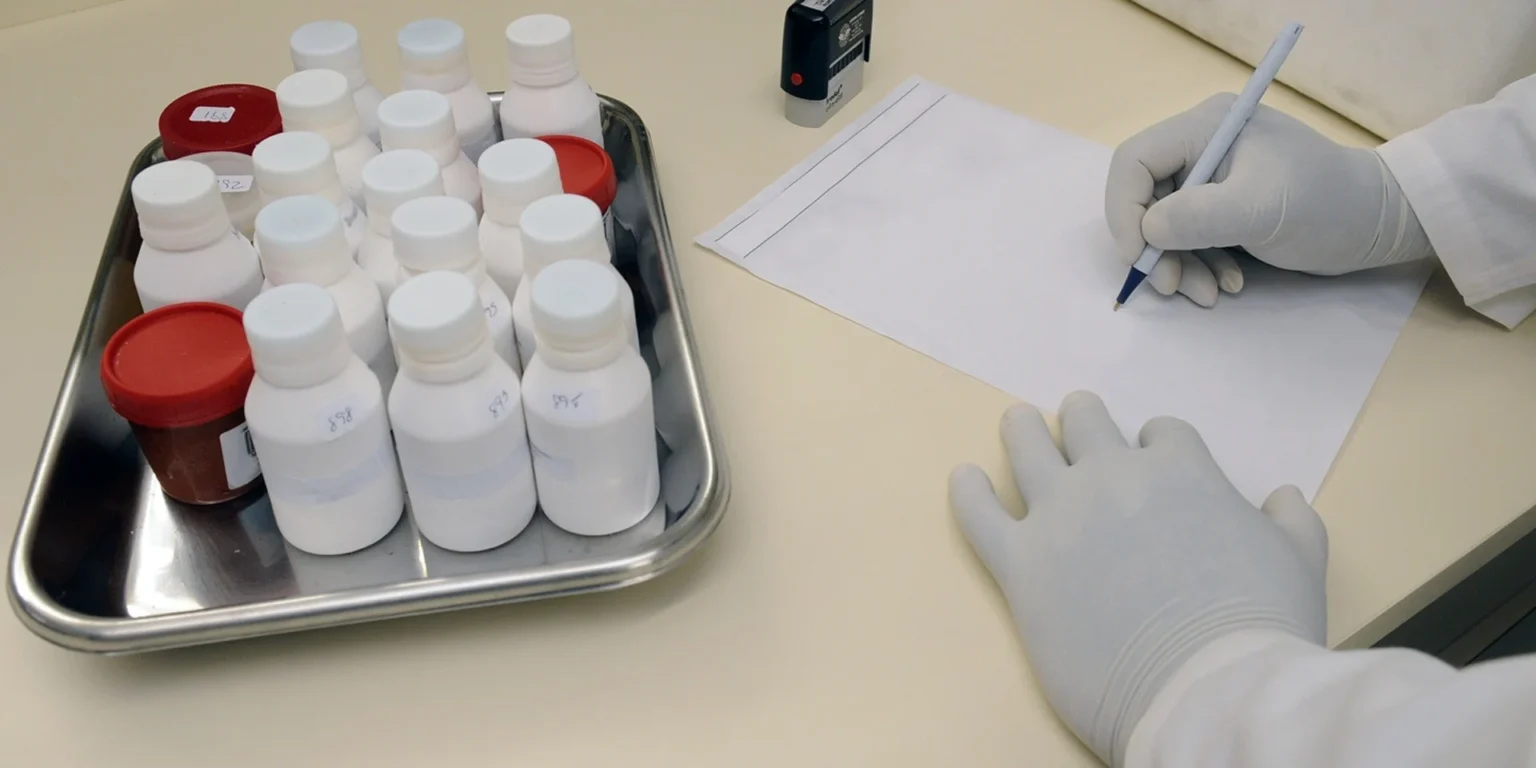
All medications don’t always suit every patient. A compounding pharmacy combines, mixes, or alters medications to tailor fit a patient in situations where, for some reason, a common medication won’t do. Some patients may be allergic to an ingredient in the medication and a compounding pharmacy can alter the medication to eliminate that ingredient. Where a patient, perhaps an elderly person or a small child, may be unable to swallow a pill, a compounding pharmacy can create the medication in liquid form to allow the patient to take the medication more easily. A compounding pharmacist can also add flavoring to a bad-tasting medication, or create a child-size dosage of a medication that’s only manufactured in an adult dosage.They can even make a topical form of a medication, such as a cream or gel, that would allow the medication to be absorbed through the skin. In some cases, where a drug manufacturer may discontinue a drug, a compounding pharmacy may be able to duplicate that medication on a small scale for patients who need to continue taking it.
Recommended for you
-
Pharmacy Technician Training Program
Our 100% online accelerated Pharmacy Technician Training program makes it possible for you to train for a new career in as little as 25 weeks!
Below are a few numbers from the International Academy of Compounding Pharmacies (IACP) regarding the compounding industry:
- The compounding industry now makes up an estimated 1 to 3 percent of the U.S. prescription market, which is $300 billion overall.
- A national survey of independent pharmacists showed that 76 percent compound medications for patients.
- Virtually 100 percent of hospitals compound medications.
- Virtually all home health specialty pharmacies compound.
- All nuclear pharmacies compound.
It is safe to assume that as long as there are patients who need specially-altered medications and doctors who rely on compounding to formulate a unique combination of medications for those patients, compounding will absolutely be necessary, as will the need for certified compounding pharmacy technician.
http://www.iacprx.org