In this blog, we’ll talk about medical billing and coding. We’ll cover what it means, the codes used, what you need to learn, how to get certified, and more. Let’s start exploring this exciting field!
What do medical billers and coders do?
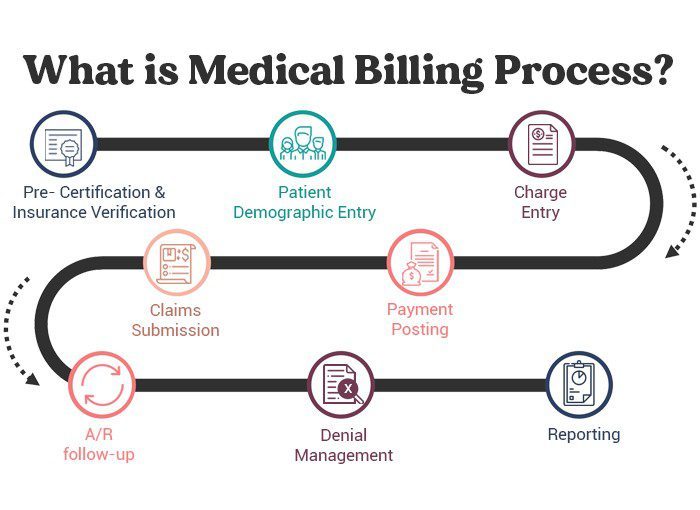
People who do medical billing and coding, also called health information technicians, have important jobs. They change medical information into codes that help with billing, insurance, and understanding statistics. Here are some things they often do:
- Look at patient records to find important information
- Give the correct codes to medical procedures, diagnoses, and treatments
- Make sure everything follows the rules and guidelines for coding
- Send coded bills to insurance companies to get paid
- Solve problems with billing and coding and fix denied claims
- Keep patient information private and secure
- Work with doctors and insurance companies to fix coding issues
To do this job well, medical billers and coders must know much about medical words, body parts, and coding systems. They also need to keep learning about changes in the industry and coding rules to do their work correctly.
Why Is Medical Billing Training Important?
Learning medical billing is essential for a few reasons:
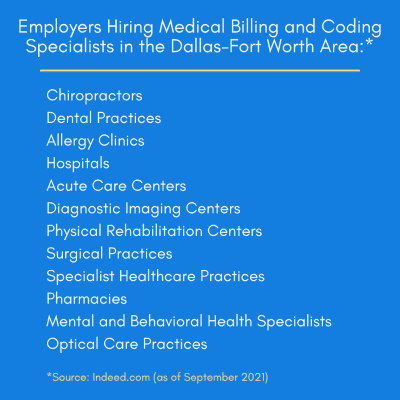
Jobs are Growing: The healthcare field keeps growing, so there are more jobs for people who know medical billing. The Bureau of Labor Statistics predicts a 8% growth in employment for medical records and health information technicians, including medical billers, from 2019 to 2029. This means that there will be ample job opportunities for individuals with the right training and qualifications.
Getting Things Right: Medical billing has many rules and codes to follow. With training, it’s easier to do it right and avoid mistakes that can cause problems. Training helps people understand these rules and do accurate billing.
Making Things Easier and Earning Money: Good billing means healthcare places run better and make more money. Training helps people do billing more efficiently, which means more money for the hospital or doctor.
What types of codes are used in medical billing and coding?
Several coding systems are used to classify medical procedures, diagnoses, and treatments in medical billing and coding. The two central coding systems are:
Current Procedural Terminology (CPT): These codes talk about what doctors do and the services they provide. The American Medical Association makes these codes used in the United States. They help figure out how much doctors get paid for different services.
International Classification of Diseases (ICD): These codes are for illnesses, injuries, and health problems. The World Health Organization makes these codes, and they are used all around the world. ICD codes make a standard way to write down and follow what’s wrong with a patient.
In addition to CPT and ICD codes, medical billers and coders may use other coding systems, such as Healthcare Common Procedure Coding System (HCPCS) codes. These codes are for medical supplies and equipment that CPT codes don’t cover.
What is involved in medical billing and coding training and education?
To become a medical biller and coder, you must learn and train. There are different ways to do this:
Vocational or technical schools: These schools have special medical billing and coding programs. You learn about medical words, body parts, coding systems, and how to handle billing and insurance. The programs usually take around nine months to 1 year.
Community colleges: Some colleges offer more extended programs, about two years. This is where you can get an associate degree in health information technology or medical coding. This gives you a more profound education, covering more than just billing and coding. It also includes other aspects of managing health information.
Online programs: If you like learning from home, online programs are available. You can study at your speed and follow the same lessons as in regular programs.
During your training, you’ll learn about medical words, body parts, coding, billing, insurance rules, and how to act ethically in healthcare. You’ll also get hands-on practice through training and internships to use what you’ve learned in real situations.
Article continues after recommendations
Recommended for you
-
Medical Assistant With Clinical Labs
Take our accelerated Medical Assistant with Clinical Labs program at our Arlington campus and start a new career in as little as 8 months!
-
Medical Assistant With Limited Radiology
Take our accelerated Medical Assistant with Limited Radiology program at our Arlington campus and start a new career in as little as 8 months!
-
Medical Billing And Coding Specialist Program
Our 100% online accelerated Medical Billing and Coding Specialist Program makes it possible for you to train for a new career in as little as 25 weeks!
-
Pharmacy Technician Training Program
Our 100% online accelerated Pharmacy Technician Training program makes it possible for you to train for a new career in as little as 25 weeks!
-
Administrative Medical Assistant Program
Our 100% online accelerated Administrative Medical Assistant program makes it possible for you to train for a new career in as little as 6 months!
What is the process for obtaining medical billing and coding certification?
While you only sometimes need certification to be a medical biller and coder, having it can make it easier to find a job and earn more money. Different groups offer certificates, including:
American Academy of Professional Coders (AAPC): They have the Certified Professional Coder (CPC) certification. It shows you know a lot about coding systems. To get certified, you must pass the CPC exam, which checks if you understand coding rules, guidelines, and medical words.
American Health Information Management Association (AHIMA): They offer two certifications, the Certified Coding Associate (CCA) and the Certified Coding Specialist (CCS). These focus on ICD coding. The CCS is more advanced and is suitable for experienced coders.
National Healthcareer Association (NHA): They have the Certified Billing and Coding Specialist (CBCS) certification. This one covers both medical billing and coding. The exam tests if you understand medical words, coding systems, billing, and insurance rules.
To prepare for these exams, you can take special courses that cover what’s in the exams and give you practice questions. Look at what each certification needs and pick the one that fits your goals and what you like.
What certification exams are available for medical billing and coding, and how can one prepare for them?
If you’re thinking about getting certified in medical billing and coding, there are some exams you can take. Here are a few well-known ones:
Certified Professional Coder (CPC) exam: This one, from the American Academy of Professional Coders (AAPC), checks what you know about CPT, ICD, and HCPCS coding. It’s a test with multiple-choice questions focusing on coding rules, guidelines, and medical words.
Certified Coding Associate (CCA) exam: The American Health Information Management Association (AHIMA) offers this one about ICD coding. It looks at your knowledge of ICD coding rules, body parts, medical words, and your coding accuracy.
Certified Coding Specialist (CCS) exam: Also from AHIMA, this one is more advanced and suitable for experienced coders. It covers ICD coding and other advanced coding things like outpatient coding, inpatient coding, and how payment works.
Certified Billing and Coding Specialist (CBCS) exam: Offered by the National Healthcareer Association (NHA), this is about billing and coding. The exam checks if you understand medical words, coding systems, billing rules, and how insurance works.
To get ready for these exams, you can use different resources:
Study guides: Many groups offer guides that cover what’s in the exam and give you practice questions. These guides help you get used to the test format and see where you need more study.
Online courses and webinars: You can find classes and webinars online that help you prepare. They often include videos, quizzes, and practice tests to reinforce what you know and improve your test skills.
Practice exams: Taking practice tests is an excellent way to see if you’re ready and figure out what areas you need to work on. Many websites have practice exams like the real ones so that you can get used to the format and how much time you have.
Networking and study groups: Joining groups of people who are also preparing can be helpful. You can share materials, talk about tricky things, and work on practice questions together.
Remember, planning enough time to prepare for the exam is essential. Make a schedule to review regularly and practice a lot. Doing this consistently will boost your chances of doing well in the certification exams.
Final Thoughts
Medical billing and coding are crucial for ensuring doctors and hospitals get paid correctly and on time. To do this job well, you need to understand medical words, body parts, and how to use coding systems. You also have to follow the rules and guidelines for coding.
Getting the proper training to work in medical billing and coding would be best. You can attend a vocational or technical school, community college, or online classes. These programs teach you everything you need to know about billing and coding. Getting certified is also a good idea because it can help you find better job opportunities and earn more money.
CCI Training Center is an excellent place to get this training. They have programs that cover all you need to succeed in medical billing and coding. They even offer courses to help you get ready for certification exams.
If you’re ready for an exciting medical billing and coding career, consider joining CCI Training Center. They can help you take the first step towards a rewarding job in healthcare administration. Start your journey today!